Tonsillitis
Written by Dr Claudia Pastides, 1st February 2019
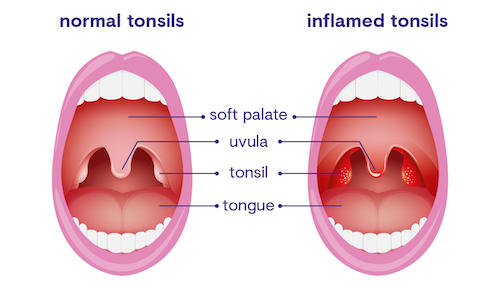
Tonsillitis is a common, often viral, infection of the tonsils that causes a very sore throat.
Around 30% of adults will suffer with a sore throat every year1, however not all sore throats are due to tonsillitis.
Is it tonsillitis or something else?
The best way of diagnosing if your sore throat is tonsillitis or not is by having a look at the back of your throat and seeing if the tonsils look red, swollen and occasionally they might have pus on them too.
Other common causes of a sore throat include:
- The common cold (often accompanied by a runny and/or blocked nose and cough)
- The flu (fever, muscle aches, headache, weakness and tiredness)
- Infectious mononucleosis/ Glandular fever (typically a high fever and swollen neck glands that last longer than a few days)
- Hand, foot, and mouth disease (usually in children under the age of 4 and presents with a fever and little blisters on the palms and soles)
When to call or see a GP
Between 60% and 85% of tonsillitis is caused by a virus. The remaining cases of tonsillitis are bacterial (often due to a bacteria called streptococcus).
Regardless of whether your tonsillitis is caused by a virus or bacteria, if you are otherwise normally fit and well – you should be able to clear the infection with the help of your own immune system and without antibiotics.
Sore throats will resolve within 3 days in 40% of people, and within 1 week in 85% of people, irrespective of whether or not the sore throat is due to a bacterial streptococcal infection2.
The complications of not having antibiotics for a streptococcal tonsillitis are very rare however it is important to be aware of the following:
- Middle ear infection (ear ache)
- Peri-tonsillar abscess (typically one-sided, worsening sore throat)
- Scarlet fever (swollen red tongue, rash on cheeks and body)
If you notice any of the above symptoms, it is important to see a GP.
Other indications of when you would need to see a GP include:
- Your sore throat is getting worse as opposed to better after 3 days
- The pain is hard to manage using over-the-counter medication
- You are feeling too unwell to carry on with regular activities
Make sure to seek urgent medical advice if:
- It becomes difficult to swallow liquids or saliva
- You are having difficulty breathing
- You have a swelling in one side of your neck
What will the GP do for tonsillitis?
If you see a GP for your sore throat, there is no secret around how they will decide whether your infection is bacterial or more likely to be viral. Of course there will always be some clinical judgement thrown into the mix, but on the whole your doctor will take a history, examine you and then use one of the following evidence-based tools to help them make the decision of whether your sore throat is more likely to be due to streptococcus or not:
- The FeverPAIN criteria
- Centor criteria
Occasionally the GP might take a swab of your tonsils, however this is rarely done as it is not usually helpful in guiding the treatment of your tonsillitis. The most important thing is your symptoms, how your body is fighting the infection and whether you are someone at higher risk of complications from tonsillitis, for example:
- the very old or young
- people who are at risk of immunosuppression
To speak to one of our GPs, download the app and create an account today.
Treating tonsillitis
The recommended treatment will vary depending on your symptoms, however the following measures (that your can carry out yourself at home) will be useful for most people:
- Make sure you keep well hydrated
- Ibuprofen and paracetamol (if not contraindicated) can help with the pain and also reduce a fever
- Gargling salt water or sucking on throat lozenges can provide some temporary pain relief
What antibiotics might I be given?
If the GP decides to prescribe you antibiotics, they are likely to be phenoxymethylpenicillin (Penicillin V), clarithromycin (if penicillin allergic) or erythromycin (if pregnant and penicillin allergic)2.
Make sure to complete the full course as prescribed and if you are not improving after 2 or 3 days, speak to a GP again.
Do I need surgery (a tonsillectomy)?
Once upon a time, tonsillectomies in childhood were very common. Nowadays tonsillectomies are reserved for people with severe recurrent tonsillitis (more than 7 episodes per year for one year, 5 per year for 2 years, or 3 per year for 3 years) or other indications, such as difficulty breathing.
This is partly to avoid unnecessarily exposing people to the (albeit low) risks of surgery, partly because tonsillitis tends to improve with age regardless and also because the evidence suggests it could cause more harm than good. For example a 2018 study of nearly 1.2 million children found that tonsillectomy in childhood was associated with a significant increase in respiratory, allergic, and infectious diseases later in life3.
References
- Kenealy T. Sore throat. BMJ Clin Evid. 2011;2011:1509. Published 2011 Jan 13.
- NICE CKS https://cks.nice.org.uk/sore-throat-acute#!topicSummary [accessed 30/1/2019]
- Byars SG, Stearns SC, Boomsma JJ. Association of Long-Term Risk of Respiratory, Allergic, and Infectious Diseases With Removal of Adenoids and Tonsils in Childhood. JAMA Otolaryngol Head Neck Surg.2018;144(7):594–603
The information provided is for educational purposes only and is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Seek the advice of a doctor with any questions you may have regarding a medical condition. Never delay seeking or disregard professional medical advice because of something you have read here.